Claim Reporting
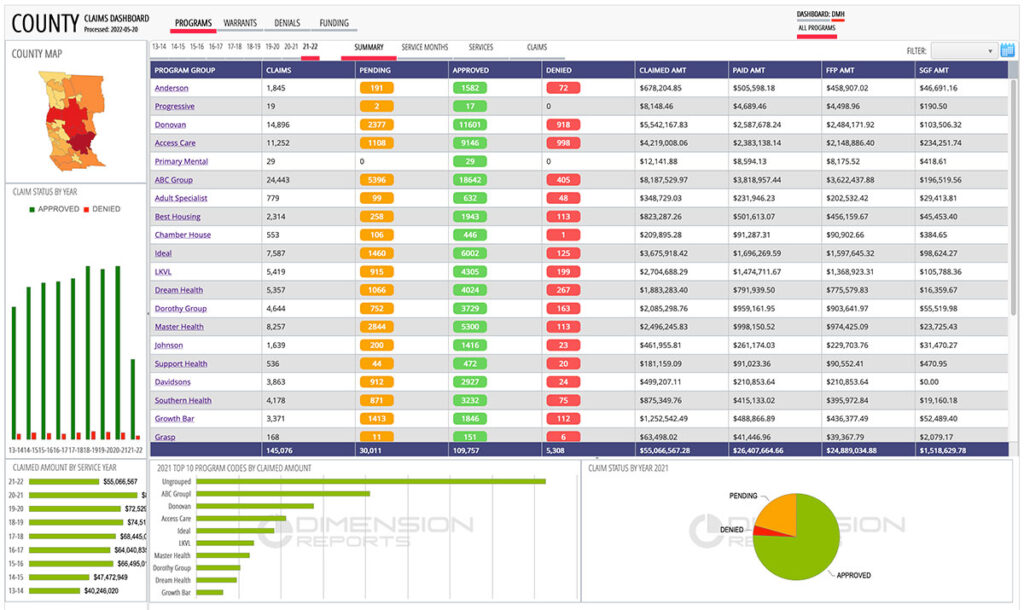
Dimension Reports DR-CLAIMS provides comprehensive reporting on Mental Health and Substance Abuse services for Medi-Cal and Medicare, resulting in billing efficiency and speedier provider reimbursements.
Full Claim Lifecycle
Track billing efficiently as claims transition from pending to approved or denied, and access key reports to identify when claims need to be rebilled or voided (screen capture).
Payment Tracking
Our advanced Medi-Cal and Medicare business rule engine simplifies reconciliation, cost reporting, auditing, and rebilling by identifying paid, unpaid and underpaid claims (screen capture).
Faster Rebilling
By identifying denials and providing clear textual denial descriptions, time-sensitive rebilling becomes fast and efficient, resulting in improved approval ratio (screen capture).
Status Requests
With status requests for outstanding claims and subsequent responses reported, following up on claims awaiting remittance is easy (screen capture).
Summaries and Details
With a clear, interactive, and visual interface, claim lines are grouped by facilities and service types, providing summaries and detailed claim line views grouped by fiscal years. (screen capture).
Rapid Deployments
Using existing 837/835 HIPAA Transactions and deploying Software-as-a-Service, the report solution can be ready for use within a matter of weeks.
Questions on Claim Reporting?
We can be reached by email at info@dimensionreports.com or by phone at 916-524-8080.
Features
Fiscal Year Breakdown
Data is organized by service or payment years allowing analytical versatility (screen capture).
Pending/Approved/Denied Claim Tracking
All clams have a rolling status based on their lifecycle (screen capture).
Warrant/Remittance Information
Identify claims and paid amounts tied to individual warrants (screen capture).
Replacement/Void Tracking
Claims requiring rebilling are clearly labeled as replacements or voids (screen capture).
Denial Reasons
All HIPAA denial codes are cross-walked into a textual description of the denial reason (screen capture).
Pending Claim Requests
Provide requests for pending claims and receive the adjudication status (screen capture).
Fund tracking
Track reimbursement from different funding sources, such as Federal Medicaid (FFP), State General Fund (SGF) and/or County funds (screen capture).